Knee pains are intolerable, and they make people unable to walk, climb stairs, or even sit. Many patients experience such problems due to knee osteoarthritis or severe injuries. Other options such as medication, injections, and others fail, so there is knee replacement surgery as an option.
What’s this idea of Knee Replacement Surgery, and who needs it? In this guide, we will break down everything you need to know, from types of surgery to recovery and long-term benefits.
What is Knee Replacement Surgery?
Knee replacement, commonly known as knee arthroplasty or total knee replacement, is a complex surgical procedure to resurface a knee damaged caused due to arthritis. Inmost of the cases a Metal and plastic parts are used for the procedure that caps the ends of the bones that form the knee joint, along with the kneecap. This surgery may be considered for someone who has severe arthritis or a severe knee injury. Below are a few things that you should know when you plan for a knee replacement surgeries
Who Needs Knee Replacement Surgery?
Knee replacement surgery may be indicated if knee pain and stiffness are likely to severely curtail your ability to carry on your activities and other failed treatments. Most people who undergo this procedure suffer from advanced osteoarthritis, which has worn away the cartilage in the knee joint.
Any of the following may make you a candidate for knee replacement surgery:
- Persistent Pain: When the pain does not subside even at rest or during nighttime, surgery might be in the cards.
- Find It Hard Moving About: Severe pain or stiffness from arthritis that renders movement impossible or extremely difficult, such as walking, climbing stairs, or getting out of and into chairs, may indicate advanced joint damage.
- Poor Quality of Life: If the pain and stiffness interfere with your ability to go about your normal daily activities, it may be time for a knee replacement.
- Swelling and stiffness: This cannot be normalized with rest; any given medication might necessitate surgical intervention. Discuss surgery with your physician as an appropriate course of action.
Stages of Knee Osteoarthritis (OA)
Stage 0: Normal: It indicates “normal” knee health where the knee joint shows absolutely no signs of OA and the joint functions without any impairment or pain.
Stage 1:Minor: The presence of a few Bone spurs which are bony growths that develop where bones meet each other in the joint. This can be presented with minor loss of cartilage but not enough to compromise the joint space.
Stage 2: Mild: X-rays of knee joints in this stage will show greater bone spur growth, however, the cartilage usually still remains at a healthy size. The space between two bones is normal, and the bones aren’t rubbing or scraping against one another.
Stage 3: Moderate: The cartilage between bones shows damage, and the space between the bones begins to narrow. Patients experience frequent pain when walking, running, bending, or kneeling.
Stage 4: Severe: Patients experience great pain and discomfort when they walk or move the joint owing to the dramatic reduction in the space between the bones
Types of Knee Replacement Surgery
Different types of knee replacement surgeries are available, depending on your condition and the extent of damage to the knee joint. Here are the main types:
- Total Knee Replacement (TKR): This is the most common form of knee surgery. The surgeon replaces the damaged surfaces of the thigh bone and shin bone with metal and plastic implants, resurfacing the entire knee joint.
- Partial Knee Replacement (PKR): If only one part of the knee is damaged, a partial knee replacement might be an option. It involves resurfacing only the affected area rather than the entire knee, preserving more of the natural joint.
- Knee Cap Replacement (Patellofemoral Arthroplasty): This type of surgery is focused on replacing only the under-surface of the kneecap and its groove, which may be the source of your pain if arthritis is limited to that area.
- Revision Knee Replacement: Sometimes, a knee replacement may wear out or fail over time. Revision surgery replaces the old implant with a new one.
The surgery choice depends on the damage’s severity and the patient’s lifestyle. Your doctor will recommend your best approach based on your needs.
Recovery After Knee Replacement Surgery
Day 1– Within the first 24 hours, your Physiotherapist (PT) will help you to stand up and walk with the help of an assistive device which can be walkers, crutches, and canes.
Day 2– On the second day, you will be made to walk for brief periods using an assistive device. As you recover from the surgery, your activity level will be increased gradually.
Discharge day: By now your knee should be getting stronger and you’ll be able to stand with minimal or no help, go on longer walks outside your hospital room, get dressed, shower, and use the toilet on your own, maybe climb up and down a flight of stairs with help
Week 3: Your pain levels would have reduced and you should be able to move around more freely. You’ll require a mild dose of pain medications.
Week 4-6: If you’ve religiously followed your rehab schedule and exercise chart as suggested by your physiotherapist, you will notice a dramatic improvement in your knee, including bending and strength. The swelling, pain and inflammation should also have gone down.
Week 7-11: Your physiotherapy and exercise regimen will continue up to 12 weeks. You will focus more on improving your mobility and range of motion and at the same time increasing strength in your knee and the surrounding muscles.
Week 12: At this point, you should have much less pain. However, you should avoid high-impact activities or high-intensity workouts that could damage your knee including the surrounding tissues. A few examples of such activities are running, aerobics, skiing, basketball, football, high-intensity cycling
Week 13 and beyond: Your knee will keep on improving and gradually over a period of time pain will reduce too. There’s a 90 to 95 percent chance that your knee will last for a minimum period of 10 years, and an 80 to 85 percent chance it will last 20 years.
Long-Term Benefits of Knee Replacement Surgery
Knee replacement surgery will also provide excellent long-term benefits that improve your quality of life. Here’s how:
- Pain Relief: Knee replacement surgery benefits typically happen through instant remedies for chronic knee pains. Most patients have seen a significant decrease in discomfort that can be borne fairly quickly, thus becoming able to continue their daily activities without much inconvenience.
- Improved Mobility: In most cases, after recovery, the patient will have a broader range of motion and can walk around free of stiffness, which previously had to limit them.
- Improvement in quality of life: With improved mobility and much less pain, you can be back doing things you love or enjoy, such as walking, swimming, or even practicing light sports. Many patients can easily return to an active lifestyle much better than before surgery.
- Long-Term Success: Most modern knee replacements are very successful. There is a 15 to 20-year period of being pain-free and stable with an appropriately placed implant.
- Less use of medications: Many patients after surgery discover they no longer need the painkillers and anti-inflammatories they were once taking before the surgery.
Why You Should Not Delay Surgery?
Patients often delay knee replacement surgery because of two significant reasons, firstly due to fear and secondly due to the apprehensions about the recovery process. While many people worry about the after-effects of the surgery, few put it on hold, thinking about what probably may happen if they wait. Below are a few consequences of the same
- Increased knee pain
- Compromised mobility and ability to use the knee
- Knee deformity, therefore harder to replace
- Further degenerative changes to the joint
- Kneecap resurfacing may be required
- Unnecessarily complications. For instance, in early intervention, a patient may only need a “partial”
knee replacement, but prolonged waiting may lead to “total” knee replacement — which is a more complex procedure.
FAQ’s about Knee replacement surgery
When do I have to get admitted to the hospital and what happens after that?
You would be admitted to the hospital on the evening before the day of the operation. Certain tests and examinations will be done to ensure that all the parameters are well in control to undergo the operation.
What kind of anaesthesia would be used for the operation?
Knee replacement surgery is usually performed under Spinal Anesthesia and Epidural Analgesia. It works by numbing your legs so that you do not feel the operation. You will also be administered medications that will help you relax and fall asleep, but you will still be able breath on your own
How long does the surgery last?
The procedure of Knee replacement usually requires 45 minutes to 1 hour. However, preoperative preparation and certain procedures after surgery will make your stay in the operation room for about two-to two-and-half-hour.
Would I require a blood transfusion during or after the operation?
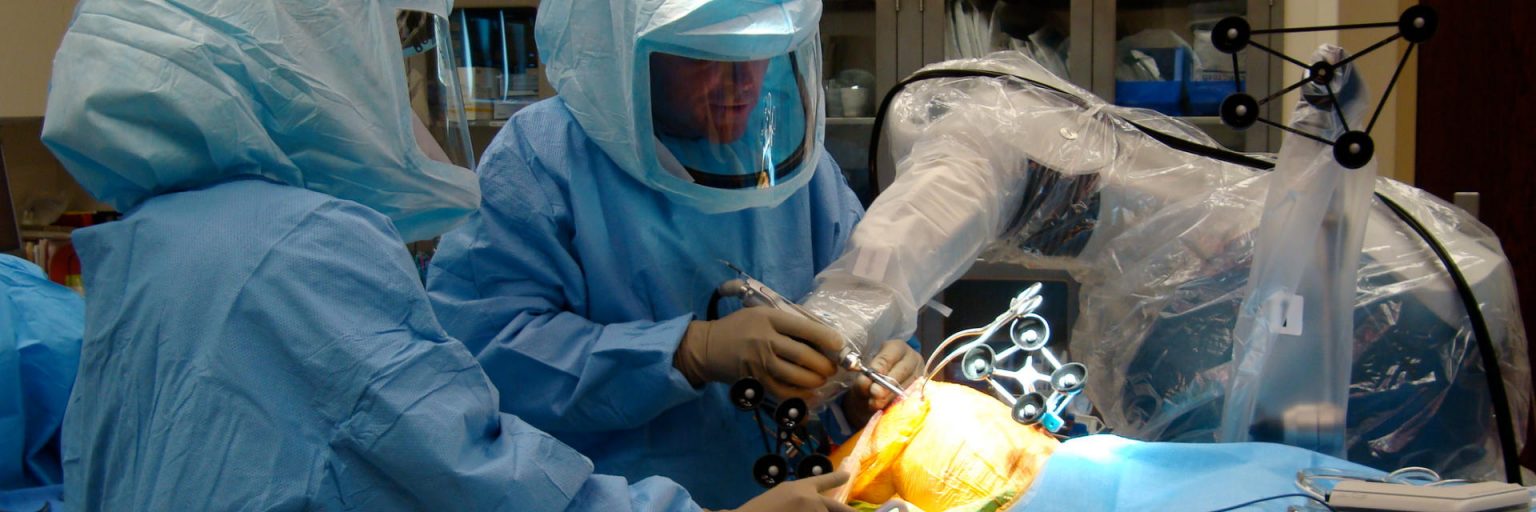
Robotic Knee replacement reduces the blood loss by precise incision and minimal tissue damage. In addition to this with use of a tourniquet, blood loss during surgery is further reduced. So during surgery, usually blood transfusion is not needed.
Will I need to go for physiotherapy and how painful is that?
Physiotherapy is the most integral and unavoidable part of knee replacement surgery. Nothing like “No Physio Knee Replacement” exists. A mild to moderate level of discomfort will be there during the initial stages of your rehabilitation. However, if you diligently follow the post-operative rehabilitation regimen and your exercise schedule you will reap long term benefits.